Transforming Heart Failure Care: POCUS-CARE Case Study Shows Significant Cost Reduction and Multi-Day LOS Savings
September 5, 2025



Background
This report presents the results of a groundbreaking Quality Improvement (QI) initiative conducted by Rutgers Robert Wood Johnson Medical School and Robert Wood Johnson University Hospital in collaboration with Butterfly Network. The study—the POCUS-CARE Trial—evaluated the integration of handheld point-of-care ultrasound (POCUS) into routine inpatient workflows for patients admitted with undifferentiated dyspnea, including congestive heart failure (CHF).
Dyspnea is one of the most common reasons for hospital admission, and CHF alone accounts for over one million U.S. hospital stays each year. The resulting burden to health systems is clinical, operational, and financial: high morbidity and mortality, persistent bed-occupancy pressure, and financial penalties tied to hospitalization and readmission rates.
Conventional workflows rarely include daily, real-time bedside imaging of cardiac and pulmonary status. The POCUS-Care Trial addressed this by equipping hospitalist rounding teams with Butterfly iQ+/iQ3 devices and training them in a mentored pathway for skills acquisition, with the support of POCUS-trained sonographers and Level 3 cardiologists. The trial was implemented using a six-month stepped-wedge cluster-randomized design across five internal medicine teams, reflecting real-world hospital conditions.
Importantly, the results of this work have been peer-reviewed and accepted for publication in JAMA Network Open, underscoring its clinical and scientific significance.
Impact
The trial demonstrated substantial clinical, operational, and financial benefits from implementing a collaborative, hospitalist-driven POCUS model:
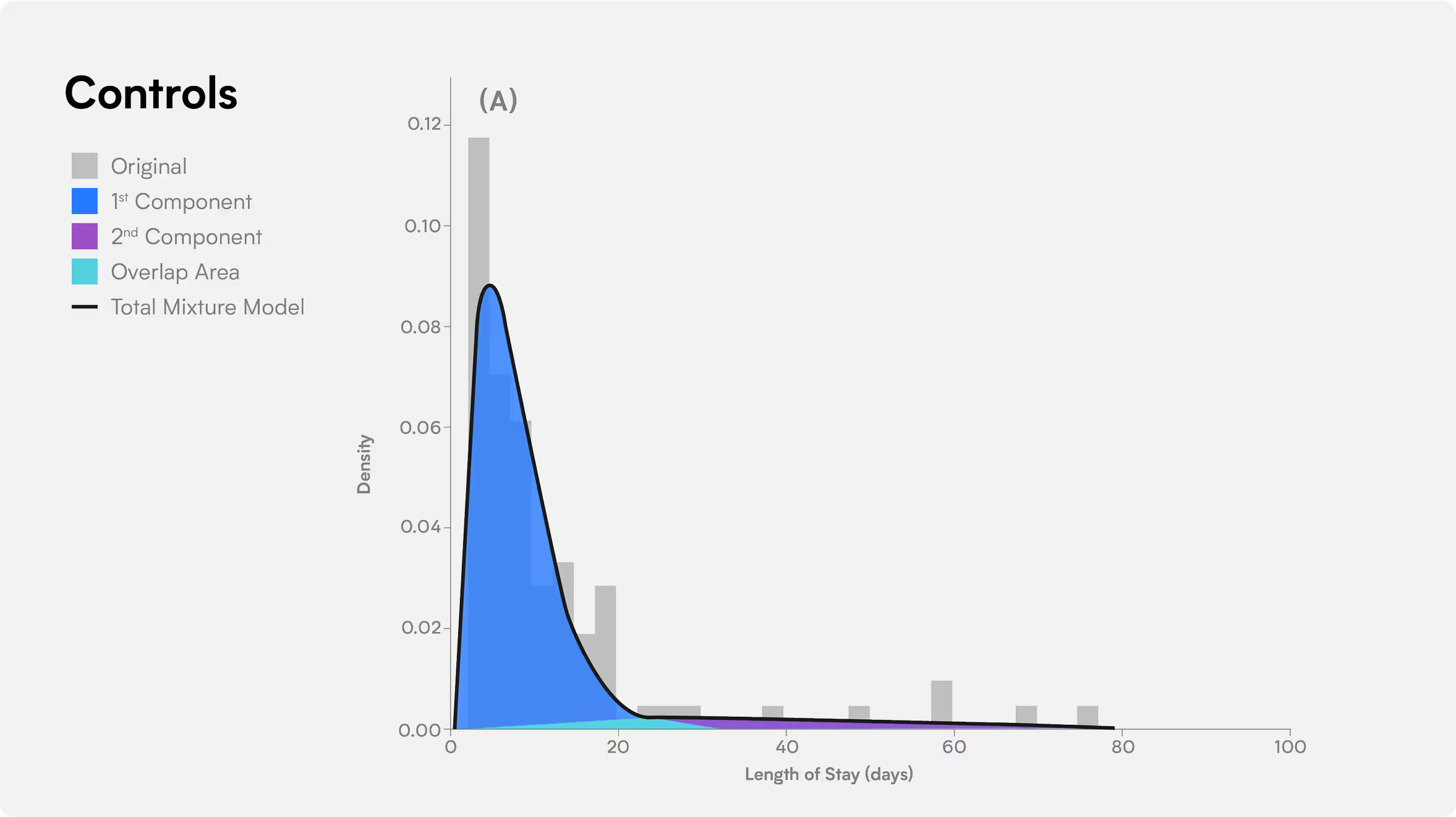
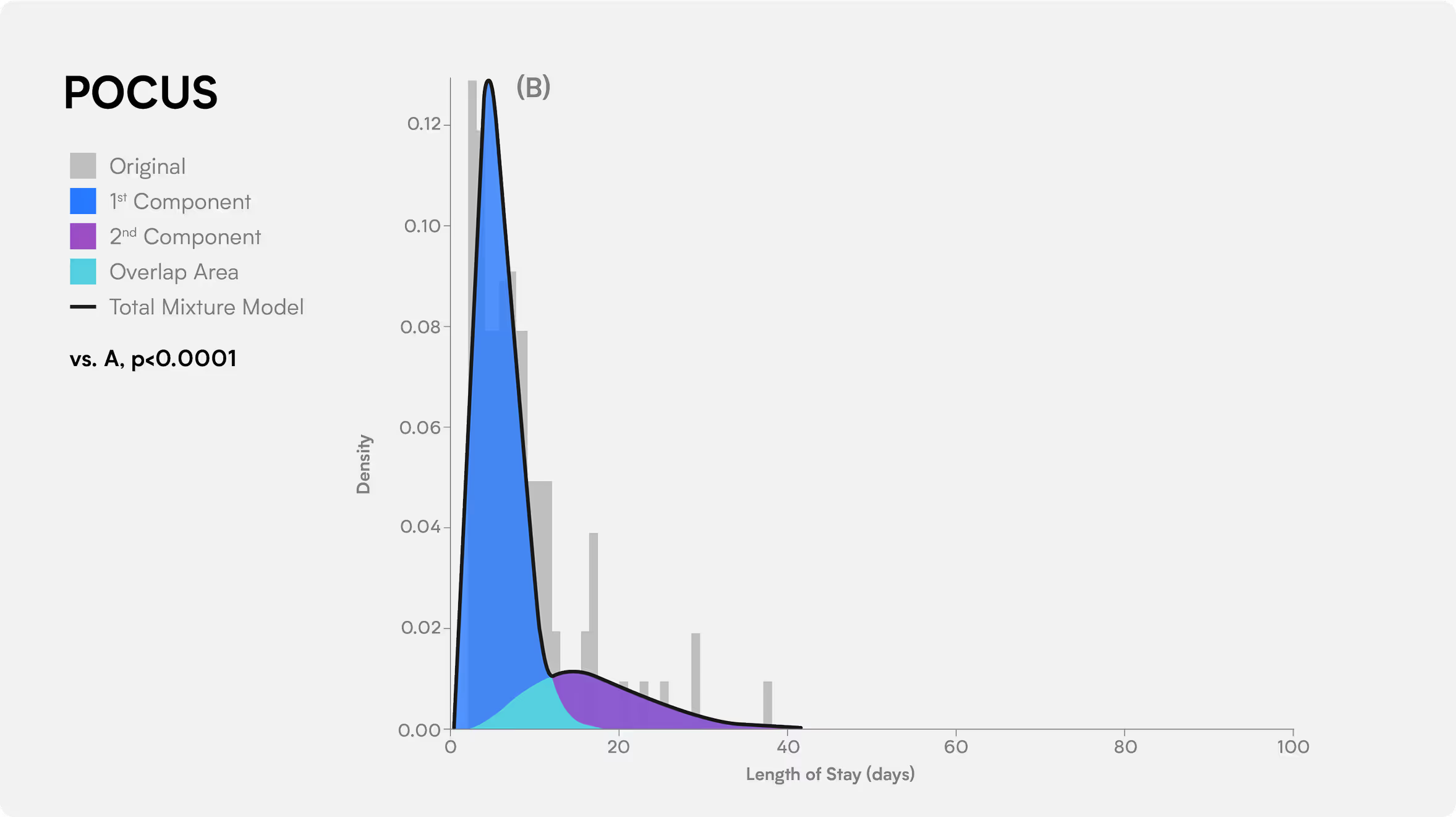
- Overall Length of Stay (LOS) Reduction:
- ~30% median reduction (11.9 → 8.3 days)
- Lower-Acuity Patients (LOS):
- 0.83–1.1 day reduction, with faster discharges largely enabled by lung ultrasound assessments
- Higher-Acuity Patients (LOS):
- 15.9–22.3 days reduction, driving the largest operational gains
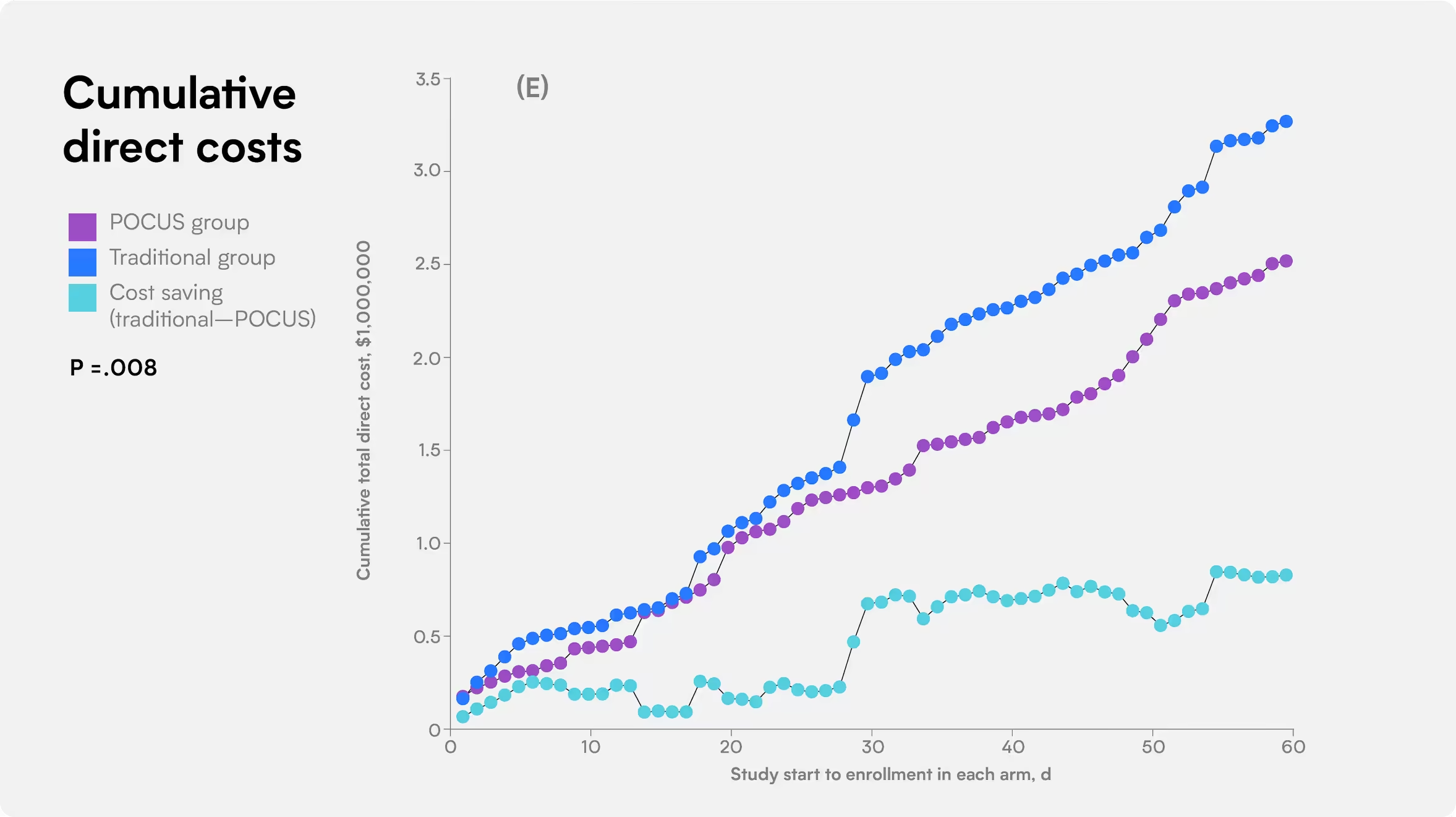
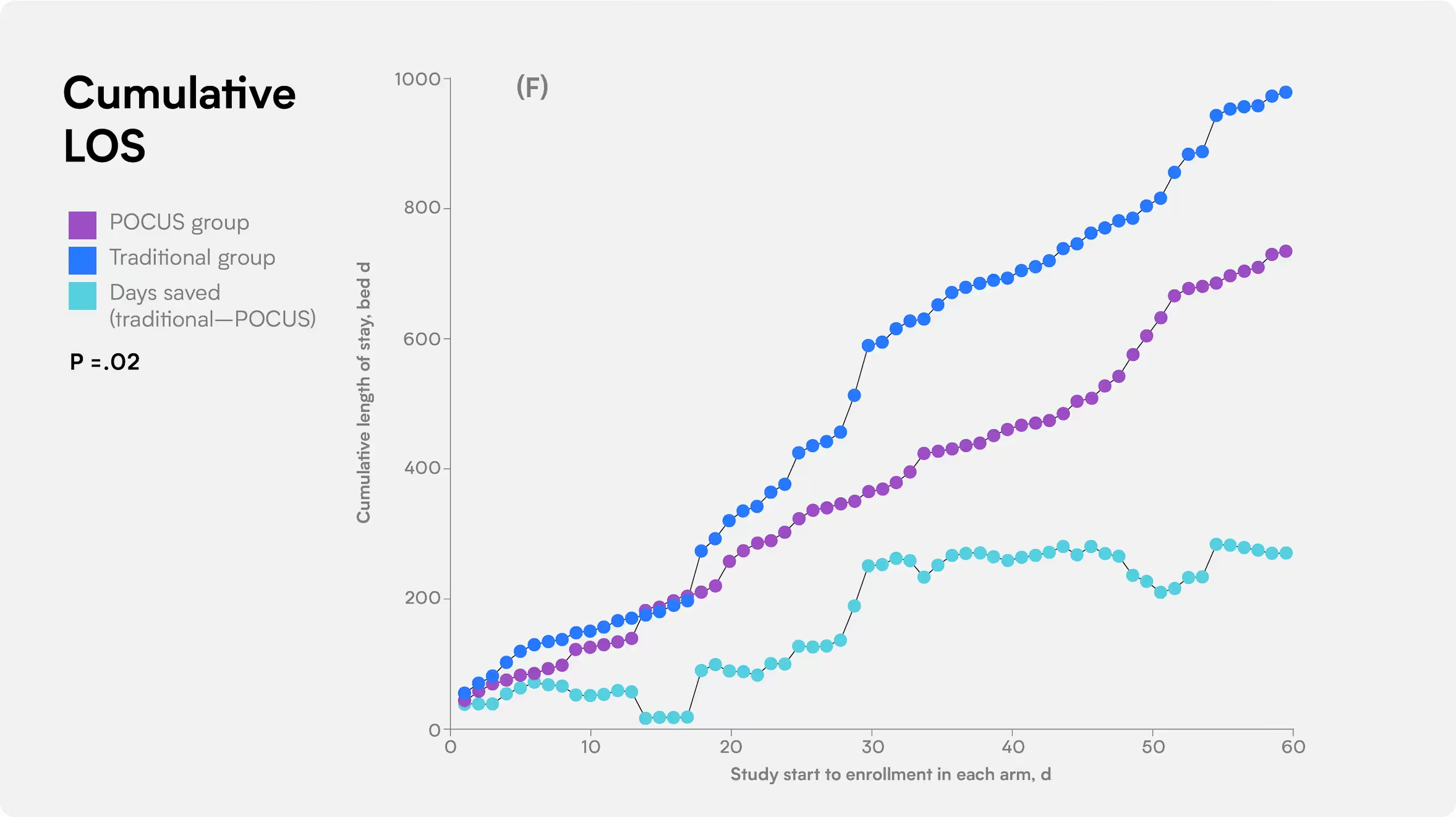
- Cumulative Bed-Days Saved:
- 246 over the study period
- Direct Cost Saved:
- $751,537 (~$3,055 per hospital bed-day saved)
- 90 Day Readmission Rate:
- POCUS group 17% versus 23% for usual care
These findings suggest that POCUS not only improves patient outcomes but also creates measurable health-system value by expanding inpatient capacity and reducing costs.
Implementing POCUS as a standard of care for CHF management has proven not only to improve patient outcomes but also to generate significant cost savings for our hospital system.
Conclusion
The Rutgers and RWJBarnabas Health POCUS-CARE Study demonstrates that integrating handheld cardiopulmonary POCUS into standard hospitalist workflows results in shorter hospital stays, fewer cumulative bed-days, and lower direct costs—yielding approximately $3,055 saved for each bed-day of capacity created.
Now published in JAMA Network Open, these peer-reviewed findings provide strong validation of a scalable, efficient model for hospitals seeking to improve inpatient CHF care while generating a clear return on investment (ROI).

